What happens to the temporomandibular joint in malocclusion
The temporomandibular joint (TMJ) is a complex anatomical system responsible for the mobility of the lower jaw: chewing, speech, yawning, and facial expressions. It functions like a hinge, ensuring smooth and symmetrical opening and closing of the mouth. However, even a minor deviation in the bite can disrupt the biomechanics of this joint.
The most common cause of TMJ dysfunction is distal displacement of the lower jaw. In this case, the mandibular condyle shifts backward relative to the articular fossa of the temporal bone. This displacement disrupts the physiological position of the intra-articular disc, which acts as a cushion between the bony structures. The result is compression of the disc, impaired mobility, and possible displacement.
Already at this stage, patients may notice a slight clicking sound when opening the mouth, often ignoring it. However, this is the first signal that the joint is no longer functioning normally.
If no intervention is made, the load on the joint begins to redistribute unevenly, triggering a cascade of microtraumas, inflammation, and deformation. The longer the incorrect jaw position persists, the higher the risk of degenerative changes in the soft and bony tissues of the TMJ.
Why ignoring symptoms is dangerous: from clicking to osteoarthritis
Many patients perceive joint clicking or slight discomfort when opening the mouth as a minor inconvenience. However, the TMJ is not just a bone junction but a complex mechanism with a delicate balance between bone, muscle, and soft tissue structures. Dysfunction in its operation accumulates over time: what seems like a small issue today can turn into chronic pain and functional limitations tomorrow.
- In the early stages of dysfunction, clicking occurs when opening or closing the mouth—this is the moment when the intra-articular disc “snaps” back into place after displacement. At this stage, there are no bony changes yet, and joint function can still be restored with minimal measures. But if this warning sign is ignored, the situation gradually worsens.
- As the condition progresses, pain develops, along with a feeling of “locking,” difficulty eating or speaking. Patients often subconsciously avoid opening their mouths wide, which worsens muscular imbalance. Gradually, adjacent neck and head muscles become involved, leading to headaches, ear and neck pain, and a sensation of a “heavy” jaw.
- Without treatment, the joint begins to deteriorate. The disc thickens, loses elasticity, and stops returning to its place. Bone structures undergo degenerative changes—TMJ osteoarthritis develops. At this stage, there are significant mobility restrictions, chronic pain, difficulty chewing, and even changes in facial contour.
Thus, the path from a harmless click to severe joint pathology can take months or years—but it is inevitable if no treatment is initiated. Early diagnosis and therapy allow the process to be stopped and joint health restored.
Stage 1 of TMJ dysfunction
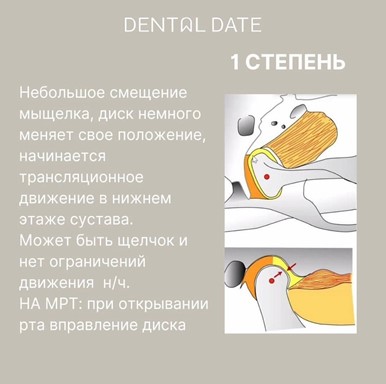
At the initial stage of TMJ dysfunction, minor anatomical changes occur, often unnoticed by the patient. The mandibular condyle begins to shift in the articular fossa, usually backward, and the articular disc slightly shifts from its physiological position.
Main symptoms:
- A short click when opening the mouth, usually painless
- Mild discomfort when chewing
- A sensation that the joint “slips,” but without restriction of mobility
- Occasional episodes of tension in the masticatory muscles
At this stage, jaw movement is generally unrestricted, and function is preserved. However, clicking during movement is already a signal that the synchronous work of the disc and condyle is disrupted.
What MRI shows
Magnetic resonance imaging reveals early discoordination between the disc and the condyle. When opening the mouth, the disc temporarily returns to place—this is the so-called “reduction,” creating the characteristic sound. Structural changes of the joint surfaces are absent, but mild stretching of the joint capsule can be seen.
Stage 2 of TMJ dysfunction

At the second stage, changes in the TMJ become more pronounced and begin to affect quality of life. The condyle displacement intensifies, usually backward and downward, causing noticeable forward and inward displacement of the disc.
Main symptoms:
- Painful clicks when opening or closing the mouth
- Episodes of jaw “locking”—inability to fully open the mouth
- Tension and pain in the masticatory muscles
- A sensation of “jamming” when eating or speaking
- Jaw fatigue by the end of the day
At this point, patients become aware that “something is wrong” with the joint, but often attribute symptoms to stress or fatigue. However, without timely correction, the ligamentous apparatus deforms, and motion mechanics deteriorate further.
MRI findings
Images show distinct forward and medial displacement of the disc relative to the condyle. In some cases, early disc deformation is visible. During jaw movement, the disc can still return to place, but this is accompanied by clicking and instability.
Stage 3 of TMJ dysfunction

At the third stage, serious structural and functional changes occur in the TMJ. The discoordination between the disc and condyle becomes persistent and obvious. Displacement of the “disc + condyle” complex progresses, and the body’s compensatory mechanisms can no longer handle the load.
Main symptoms:
- Sensation of “sticking” or locking when opening the mouth
- Constant stiffness of the jaw
- Headaches, especially in the temples and occipital region
- Dull pain when chewing, intensifying in the evening
- Discomfort in the neck area and stiffness
Patients often complain of a feeling that the jaw is “slipping out of place” or “misaligned.” A pathological movement pattern forms: the person instinctively avoids fully opening the mouth, which further aggravates functional restrictions.
MRI findings
MRI clearly shows anterior displacement of the disc, which no longer returns to its physiological position during movement. Thickening of the anterior portion of the disc indicates chronic overload. Bone structures remain intact, but signs of joint overload are visible.
Stage 4 of TMJ dysfunction
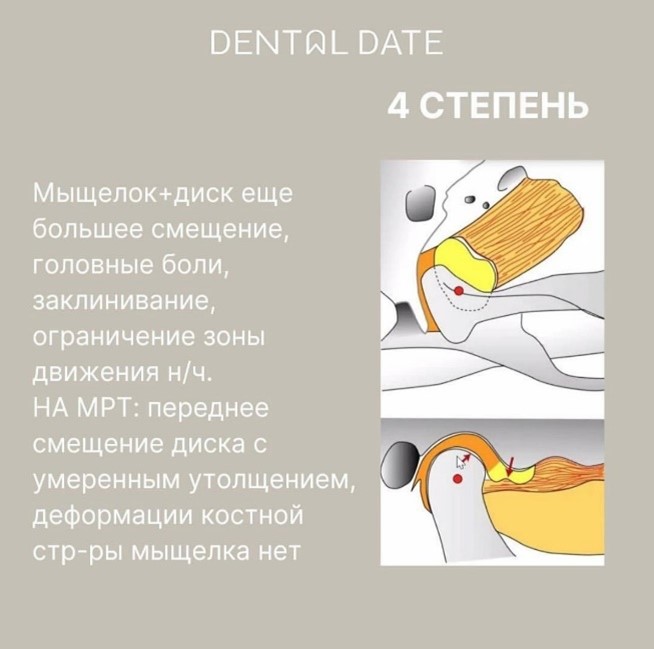
At the fourth stage of TMJ dysfunction, significant anatomical and functional disruption occurs. Pathological processes transition from the functional to the structural phase: changes in the disc and condyle become pronounced and less reversible.
What happens:
- The disc thickens, becomes less elastic, and loses its ability to move
- The mandibular condyle continues to shift backward and upward, exerting constant pressure on tissues
- Gradual destruction of joint surfaces begins—bone friction causes inflammation and pain
Clinical manifestations:
- Chronic, often throbbing pain in the ear, temple, and jaw
- Difficulty chewing, sensation of stiffness in jaw movement
- Pain worsens with talking, eating, or after stress
- Painful tension of masticatory and neck muscles
- Facial asymmetry (in severe cases)
What MRI shows
- The disc no longer returns to place when opening the mouth
- Its shape is altered: anterior thickening, posterior shortening
- Condylar contours become uneven, with early signs of bone degeneration
- Fibrous inclusions may be present in the joint space, indicating chronic inflammation
Stage 5 of TMJ dysfunction
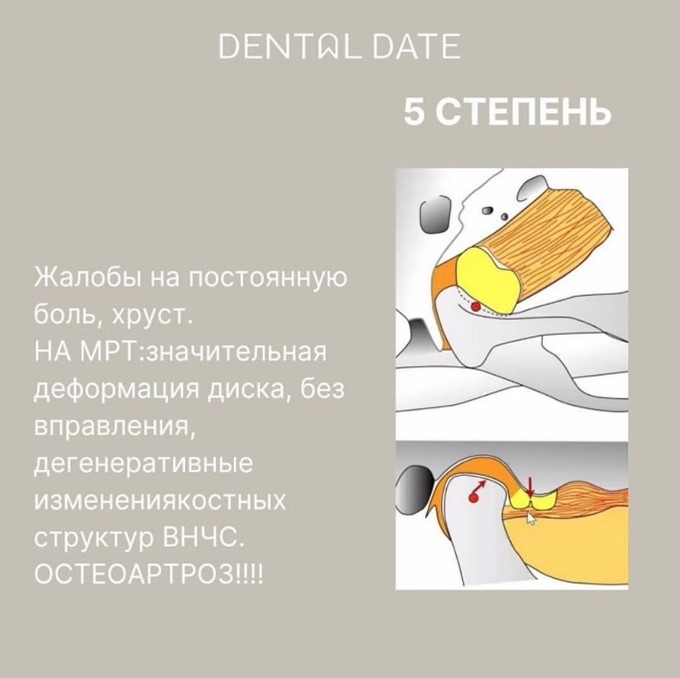
The fifth stage is the terminal phase of TMJ dysfunction, marked by severe degenerative changes not only in the disc but also in the bone tissue. At this stage, the joint can no longer function properly, and the patient’s quality of life is severely reduced.
What happens in the joint:
- The disc is completely deformed: thickened, displaced, and irreducible in any jaw position
- Degenerative changes in the condyle and articular fossa are evident: cartilage wear, areas of osteosclerosis, and osteophytes (bony outgrowths)
- Clinical picture of TMJ osteoarthritis forms—a chronic progressive disease with joint destruction
Symptoms:
- Constant dull or sharp pain, unrelated to jaw movement
- Restricted mouth opening amplitude to 20–25 mm or less
- Loud crepitus, clicks, or grinding when attempting to open the mouth
- Impaired chewing—patients cannot eat normally
- Secondary symptoms often arise: headaches, neck pain, sleep disorders, anxiety, dizziness
What MRI/CT shows:
- Clear signs of arthrotic changes: condylar flattening, deformation of the joint head, narrowing or absence of the joint space
- The disc is so altered that anatomical restoration is impossible
- Bone outgrowths, joint capsule thickening, and inflammatory changes are visualized
Why this stage is dangerous
At this point, not only the mechanics of the jaw are impaired, but also the functioning of other body systems. Chronic pain affects psycho-emotional state, while occlusal deformity can worsen facial aesthetics.
Causes of TMJ dysfunction progression
TMJ dysfunction is not just a local disorder, but the result of systemic changes that worsen over time without intervention.
Causes of progression may be anatomical or functional:
Lack of timely treatment. Early symptoms—clicks, mild discomfort—are often ignored. Without correction, the pathology progresses step by step: from minor disc displacement to irreversible joint destruction.
Malocclusion and bite pathology. Even slight mandibular displacement changes joint loading. Constant asymmetric tooth contact disrupts biomechanics and overloads joint structures.
Muscle imbalance and parafunctions. Teeth grinding, clenching habits, or asymmetric chewing create chronic muscle overstrain, provoking disc displacement and microtrauma.
Inflammatory and systemic diseases. Infections, arthritis, autoimmune conditions can provoke or accelerate degenerative joint changes.
Jaw and neck trauma. Even old, forgotten injuries (e.g., a chin bruise or facial blow) can alter TMJ biomechanics and trigger its gradual destruction.
Why early intervention is important
Early diagnosis of TMJ dysfunction is key to preserving joint health and patient quality of life.
Reasons not to delay a visit to a specialist:
- Reversibility of early changes. At stages 1–2, conservative treatment alone is sufficient: myotherapy, splints, bite correction without surgery.
- Prevention of chronic pain. Once pain becomes constant, pain memory forms. Even after treatment, the brain may continue to “reproduce” discomfort, making relief harder.
- Support of overall health. The TMJ is closely linked to posture, breathing, and even tongue position. Treating the joint restores balance in the entire body.
- Saving time and costs. Early treatment requires less time, fewer steps, and lower expense. Prevention and initial therapy are far cheaper than complex reconstructive surgeries.
Conclusion
TMJ dysfunction is not just “clicking when opening the mouth,” but a serious condition capable of altering the entire facial skeletal mechanism and causing persistent pain.
It is important to understand: the longer symptoms are ignored, the higher the risk of reaching advanced stages with irreversible changes requiring surgery. Modern diagnostics allow accurate determination of severity, and timely treatment can halt the pathological process.
Regular visits to a gnathologist, monitoring bite, posture, breathing, and muscle tone are the foundation of a healthy joint and a full life without pain or restrictions.